Prepared by Sunita Shamsul (Assistant Research Officer, SIDC).
Edited by Prof Andrew Kiyu
Summary
- Omicron 2.87.1 sublineage is cautiously tracked by South Africa, the US and scientists in Europe; its impact on disease transmission is so far low.
- Peter Sandman thinks that Covid-19 pandemic should dwindle for longer, and not be over
- The CDC unveiled a new syphilis testing guidance amid a
- The search for the best rapid test for Nipah and Lassa fever virus is
- Measles might blow out of proportion in low- and middle-income countries amid vaccine hesitancy and misinformation.
- Cholera is a serious health threat in crises-laden
- Zoonotic diseases will continue to plague humans due to the overlapping of the human- animal boundary.
1.0 Variants
1.1 Omicron BA.2.87.1, updates
The CDC has been tracking a new variant of SARS-CoV-2 named BA.2.87.1 because of “its large number of changes in the spike protein”. BA.2.87.1 has more than 30 changesFootnote1 in the spike protein compared with XBB.1.5, the variant the latest updated vaccine is designed to protect against.1 2 South Africa has identified 9 cases of BA.2.87.1 in samples collected between September to December 2023 from three provinces (no clustering) – indicating that the sublineage is not highly transmissible.3 The country has not seen any detectable increase in COVID-19 cases or deaths since the last quarter of 2023.4
1 GLOBAL UPDATES ON COVID-19 AND OTHER DISEASES (12 FEBRUARY 2024), Section 2.0 (5 February 2024): BA.2.87, has > 100 mutations compared to the ancestor Omicron variant (BA.1.1.529).
To date, other than South Africa, only two other countries have reported BA.2.87.1: the US and Italy. However, according to the Geneva Centre for Emerging Viral Diseases, one was of low quality while the other was “dubious”.5 Although BA.2.87.1 sublineage resembles the precursor to JN.1 in many ways, it needs to acquire additional mutations to increase the angiotensin converting enzyme 2 (ACE2) binding, or the population needs to develop substantial immunity against JN.1.6
According to the CDC, while it may be unclear how well the current (updated monovalent mRNA) vaccine would protect against BA.2.87.1, recent experience with the JN.1 variant suggests that the current COVID-19 vaccine can help protect against a diverse range of variants.2
2.0 Outcome
Death rates among SARS-CoV-2 variants
A meta-analysis based on global data revealed that among all the SARS-CoV-2 variants of concern (VOC) to date, Beta was the deadliest. It was followed by followed by Gamma, Alpha, Delta, and Omicron. The variant-specific case-fatality rates (CFRs) ranged from 0.7% to 4.2%.7 8
The researchers reviewed 112 epidemiologic studies on COVID-19’s CFR published from January 2020 to March 2023; 31 were from Asia, 23 from Europe, 16 from Africa, 15 from North America, 15 from South America, and 12 from Oceania. The studies were cross- sectional (62), retrospective observational (36), cohort (10), and ecological (4). The analysis found the following (paraphrased):8
- The pooled/average CFRs of COVID-19 varied across the epidemic periods of different VOCs (Table 1).
Table 1. The pooled/average case fatality rate, CFR, of different variants of concern, VOC, according to region. The table was adapted and information extracted from Case fatality rates of COVID‐19 during epidemic periods of variants of concern: a meta- analysis by continents. – International Journal of Infectious Diseases (ijidonline.com)
CFR RATES % FOR VOCs
| REGION | Ancestral | Alpha | Beta | Delta | Gamma | Omicron |
|---|---|---|---|---|---|---|
| NORTH AMERICA | 4.8 | 2.7 | – | 2.5 | – | 0.7 |
| SOUTH AMERICA | 5.5 | – | – | 2.8 | 3.6 | 0.2 |
| EUROPE | 3.2 | 1.4 | – | 1.1 | – | 0.4 |
| AFRICA | 3.0 | – | – | 3.5 | – | 1.8 |
| ASIA | 3.5 | 4.4 | – | 1.5 | – | 0.5 |
| OCEANIA | 1.8 | – | – | 2.1 | – | 1.1 |
| OVERALL | 3.6 | 2.6 | 4.2 | 2.0 | 3.6 | 0.7 |
‘ – ‘ Insufficient literature.
-
- The CFR rates for Omicron subvariants are as follows: 1.0% for BA.1, 0.2% for BA.2, and 0.4% for BA.5. Even though the CFR for Omicron is the lowest, a study published in 2023 revealed that it was still four times higher than for seasonal flu.9 10
- The CFRs of COVID-19 disparities existed among continents.
- The CFRs in Europe and North America during the Alpha’s period were lower than those during the wild-type period. The opposite was seen in Asia. This was likely due to better monitoring and testing capacity in European and North American countries in the early stages of the outbreak; able to cope in identifying severe cases which resulted in identifying more deaths caused by COVID-19.
- VOCs, Human Development Index (HDI) valueFootnote2, age, and coverage of vaccination were factors influencing the CFR.
- The proportion of study participants ≥ 60 years old and CFRs were positively correlated (Table 2).
2 According to the UNDP, Human Development Index (HDI) is “a summary measure of average achievement in key dimensions of human development: a long and healthy life, being knowledgeable and having a decent standard of living”. It was created to emphasise that people and their capabilities should be the ultimate criteria for assessing the development of a country, and not solely on economic growth.64
Table 2. The pooled case fatality rate, CFR, according to age. The table was adapted based on information obtained from Case fatality rates of COVID‐19 during epidemic periods of variants of concern: a meta-analysis by continents. – International Journal of Infectious Diseases (ijidonline.com)
| Description | Proportion, % | CFR, % |
|---|---|---|
| The proportion of study participants ≥ 60 years old | < 10 | 0.9 |
| 10 – > 20 | 2.8 | |
| > 20 | 4.7 |
-
- The pooled CFRs were 4.9%, 1.4%, and 0.6% for participants with a full vaccination rate < 30%, 30% to 60%, and > 60%, respectively.
The CFR is influenced by many factors (such as resources and policies), the combined effects of which would give outcomes specific to the context in which it is studied. Therefore, approaching the gaps in CFRs would require some caution.
3.0 Planning
3.1 CDC’s new office in East Asia and Pacific Regional Office, Japan
The CDC opened a new office in Asia located in Tokyo on 5 February 2024. It will serve as the agency’s East Asia and Pacific regional office to address health security within the region and globally “to prevent, detect and respond to health threats”. Priorities for the new regional office include (paraphrased):11
- Expanding CDC’s core global health security capacity by building stronger collaboration and partnerships in the East Asia and Pacific region,
- The ability to detect public health threats and respond quickly, and
- Knowledge and information exchange between CDC and the region.
The Agency has set up several regional offices globally to “promote the country’s health security objectives and establish a lasting global presence”.12
3.2 Why the COVID-19 pandemic should dwindle longer, and not be over yet
In January 2024, Peter Sandman, a risk communication consultant from the US gave his perspective on MedPage Today on why the COVID-19 pandemic should not be over. A summary is presented here.13
On the last day of 2023, officials from the WHO cautioned the people that the COVID-19 pandemic was far from over. As it continues to be a threat to health, there are a variety of known ways to reduce the risk of the disease. Complacency, however, is at a high level. It does not have a place in public health. While the number of COVID-19 deaths reported in the US has declined dramatically since 2020, the statistics from the first half of 2023 showed that COVID-19 is twice deadlier than the flu virus.14
The SARS-CoV-2 virus continues to evolve, the trajectory of which is unknown – whether it continues to be (perceived as a) ‘less dangerous’ version of the current lineages, or if it will make a U-turn to become a deadlier version. The parent of JN.1 variant of interest (VOI), BA.2.86 gained the same feature as previous VOIs – the ability to infect lung cells more easily via the cellular enzyme transmembrane protease, serine 2 (TMPRSS2).15 16 17
Long-COVID or post-COVID-condition still needs addressing as it affects those in the workforce and will have a significant impact on the economy of a country (sick leave, therapeutics [drugs and non-drugs]).18 19 20
Seasonal influenza, though can be serious, transmissible, and widespread, has been circulating for much longer and is somewhat ‘predictable’ – knowing what to expect so far. COVID-19 has not yet reached the seasonality or predictability of influenza. Until it does, it remains a pandemic.
Two scenarios can happen in the next few years:
- The immediate future (2024, 2025, and 2026) will turn out to be similar to 2022/2023; to deal with a new normal that includes a new disease nearly twice as deadly as the flu, in addition to the flu and all the other diseases that are currently faced.
- The number of COVID-19 cases and deaths (transmission and severity) decline and COVID-19 will have settled into a newly familiar pattern significantly less deadly than it was in 2023 and/or previous years. The disease will dwindle before it finally ends.
“More dwindling before it ends would promote better health outcomes.”
Peter M. Sandman, MedPage, 24 January 2024.
3.3 Syphilis, new testing guidance
The CDC has released the first comprehensive laboratory recommendations for syphilis testing. The new recommendations include approaches for laboratory-based tests, point-of- care tests (POCT), sample processing, and how laboratories should report test results to clinicians and health departments. The recommendations are primarily for clinical laboratory or disease control personnel. It is for clinicians to understand how to collect and process specimens, interpret test results, and counsel and treat patients.21 22
3.4 CEPI and FIND partner to identify best Nipah and Lassa virus rapid tests
The Coalition for Epidemic Preparedness and Innovations (CEPI) announced on 16 February 2024 that it is funding a 4-year project led by the Foundation for Innovative New Diagnostics (FIND) to identify the most reliable rapid tests for Nipah and Lassa virus infections.23 Both diseases are among CEPI’s priority pathogens. The group is funding work on vaccines for both diseases. Grants up to USD14.9 million will be allotted by CEPI for the rapid test project, which is expected to pave the way for licensing the tests for widespread use.24
4.0 Others
4.1 Zoonosis
4.1.1 Alaskapox fatality, Alaska, the US
The Alaska health authorities reported the first fatality of Alaskapox on 9 February 2024. The infection involved an elderly man with underlying health problems who died in late February 2024. He was suspected to have contracted the disease sometime in September 2023 whilst undergoing cancer therapy. He lived alone in a forested area in Kenai Peninsular, South- central Alaska, and did not have a history of recent travel nor close contacts with recent travellers.25
Initial laboratory test was positive for cowpox, and follow-up testing at the state health laboratories was positive for Orthopoxvirus. The CDC subsequently found the case samples to be consistent with Alaskapox virus (AKPV), though genetically distinct from earlier cases that had been reported in Fairbanks, an area in the forested interior of Alaska and > 800 km from the latest case. A stray cat that the patient had cared for, which on occasion scratched him, was negative for the virus. The patient was also reportedly gardening (being outdoors) through September 2023.
He had sought care for 6 weeks after a lesion first appeared and was subsequently hospitalised when his condition worsened. He was treated with antivirals (ecovirimat or Tpoxx, used against orthopox viruses such as mpox and smallpox; and brincidofovir, used against smallpox),26 27 and intravenous vaccinia immunoglobulin.28
Authorities noted that this case is the first outside of the state’s interior, which has suggested that AKPV is more widespread in the state’s small mammal population than previously known, and clinicians should be made aware of the situation. Epidemiologists and their health partners, including the CDC, are currently testing small mammals outside of Alaska’s interior region to gauge the prevalence of AKPV in animals.25 29
[NOTE]:
Alaskapox is thought to have first emerged in the human population in 2015 in the Fairbanks area in Alaska. It is a DNA virus belonging to the genus Orthopoxvirus whose members include cowpox, mpox, and smallpox. It can cause a fever, fatigue, and rashes/lesions on the skin.30 It is a zoonotic virus which has been linked to four small mammal species, predominantly red- backed voles. Occasional spillover into the human population is rare. There is evidence suggestive of prior AKPV infection in at least one domestic pet linked to a patient. The extent of AKPV’s geographic distribution and animal reservoirs remain unknown.31
Including the current case, 7 AKPV infections have been recorded by the Alaska Section of Epidemiology (SOE). Until December 2023, all reported infections occurred in residents of the Fairbanks area and involved self-limiting illness (not requiring treatment) consisting of a localised rash and lymphadenopathy. There is no evidence so far of human-to-human transmission of AKPV and these cases were seen in an outpatient setting. However, it was noted that other similar Orthopoxvirus can spread through contact with skin lesions. The authorities have recommended patients avoid touching rashes and sharing clothes, as well as to wash clothes and bed linens separately from other household laundry.
Current available evidence continues to suggest that the public health impact of AKPV is limited.
4.1.2 Bubonic plague: human case, the US
Oregon confirmed its first case of human plague in more than 8 years. According to health officials in Deschutes County, a rural part of the state, the disease had most likely been transmitted by a pet cat. The patient was reportedly responding well to antibiotics. As a precaution, the patient’s close contacts were given antibiotics to prevent any potential infections from developing into symptoms.32 33 34
The last case of bubonic plague reported in Oregon was in 2015 when a teenage girl “presumably” got infected from a flea bite during a hunting trip.34 According to the health authorities in Oregon, there have been 18 human cases reported in the state since 1934.35
The plague was introduced into the US in the 1900s via by rat–infested ships that had sailed from affected areas, mostly from Asia. The last urban plague reported occurred in 1925. The disease subsequently spread to urban rats and rural rodents. It became established mainly in the western part of the US. According to the CDC, there have been 496 human cases of the plague reported from 1970 and 2020. Between 2000 and 2020, 116 cases were reported including 14 deaths. Over 80% of United States plague cases have been the bubonic form.36
[NOTE]:
Plague is a zoonotic disease caused by enterobacteria Yersinia pestis. It is primarily carried by rodents and spreads to humans and other animals via fleas. Direct person-to-person transmission does not occur except in the case of pneumonic plague, when respiratory droplets may transfer the infection from the patient to others in close contact. Household pets can get also infected if they hunt rodents infected with the plague or are similarly bitten by an infected flea.36 37 They can then pass the infection to humans via tissue or bodily fluids, such as respiratory droplets from cough or sneezes. Alternatively, they might carry home fleas that, in turn, bite humans. Unlike dogs, cats are more susceptible to plague because their bodies have a hard time clearing the infection, and they’re more likely than some other pets to chase and capture rodents.33
People infected with the plague usually develop acute febrile disease with other non-specific systemic symptoms after an incubation period of one to seven days, such as sudden onset of fever, chills, head and body aches, weakness, vomiting, and nausea.37
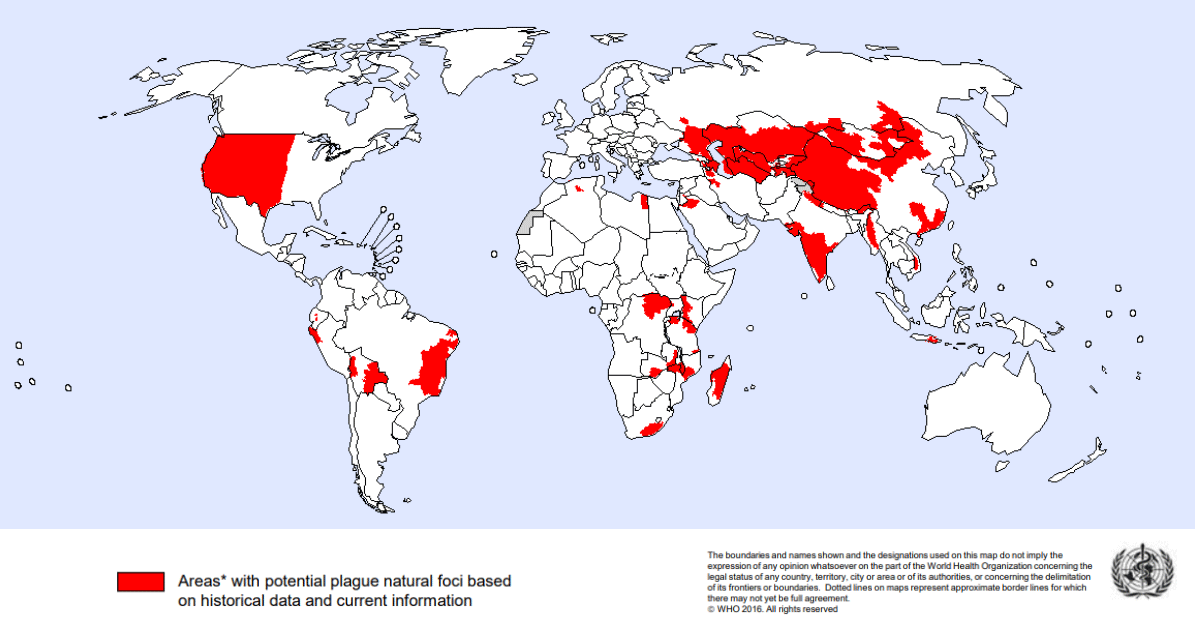
The plague is found in almost all continents, except Oceania (Figure 1). There is a risk of human plague wherever the presence of plague natural foci – the bacteria, an animal reservoir, and a vector – and human population co-exist.
Figure 1. Global distribution of natural plague foci as of 2016. There were 3,248 cases of plague reported worldwide from 2010 to 2015, including 584 deaths. The map was obtained from plague-map-2016.png (1195×625) (who.int).
Antibiotic treatment is effective against plague bacteria. Therefore, early diagnosis and early treatment can save lives. Preventive measures include informing people when zoonotic plague is present in their environment, good sanitation, and to minimise contact with infected fleas and rodents to help prevent plague pandemics.38 39
The US National Institute of Allergy and Infectious Diseases (NIAID) has classified Y. pestis as a Class AFootnote3 pathogen along with Bacillus anthracis (causes anthrax), Clostridium botulinum toxin (botulism), and viruses that cause haemorrhagic fevers.40
3 Class A pathogens are organisms/biological agents that pose the highest risk to national security and public health because they can be easily disseminated or transmitted from person to person; result in high mortality rates and have the potential for major public health impact; might cause public panic and social disruption; and requires special action for public health preparedness.40
4.1.3 Middle East Respiratory Syndrome coronavirus surveillance, Kenya
A year-long sampling of dromedary camels in northern Kenya revealed some insights into Middle East Respiratory Syndrome Coronavirus (MERS-CoV) circulation that was missing in surveillance studies. It found episodic cases of Middle East respiratory syndrome (MERS) and evidence of human infections.41
The surveillance identified biphasic (two-phase) peaks of the MERS-CoV from September 2022 to September 2023. It also identified more than three case clusters over 3 weeks in camels from different areas, as well as a 15% infection rate among slaughterhouse workers. Ten to 15 camels were sampled from 12 different regions 4 or 5 days a week during that time. The summary of the findings is as follows (paraphrased): 42
- Reverse transcription-polymerase chain reaction (RT-PCR) detected MERS-CoV RNA in 1.3% of The incidence peaked in early October 2022, at 11.7%, and in February 2023 (12.1%), corresponding to Kenya’s dry seasons when camel calves lose their maternal antibodies.
- Enzyme-linked immunosorbent assay (ELISA) of MERS-CoV immunoglobulin G antibody (IgG) levels in 369 random samples (from a total of 2,711) showed an 8% seroprevalence. It was lowest in June and highest in March. IgG levels were negatively associated with RNA positivity.
- IgG reactivity was identified in 7 of the 48 slaughterhouse workers (14.6%), with 1 of them showing evidence of MERS-CoV neutralising antibodies (nAb). None were severely ill.
Limited infrastructure in remote and resource-restricted regions can hamper field studies on nomadic camels. However, animals that are regularly transported to abattoir hubs can sustain daily testing.
The increased camel-to-camel interactions between unexposed and infected animals from different herds in slaughterhouses could have influenced outbreaks of MERS. Local risk factors such as herding practices and seasonality can also influence outbreaks. Rapid point-of-care tests could help trace infections in resource-limited conditions, such as was encountered during this study. Identifying defined factors that drive MERS-CoV outbreaks will assist in predictive epidemiology, risk assessment, and timely precautionary interventions for public and occupational health.
MERS-CoV was first discovered in humans in Saudi Arabia in 2012 and has since spread to many other countries. It is endemic in dromedary camels from the Arabian Peninsula and Africa; the seroprevalence is >75%. Zoonotic transmission to humans has occurred sporadically, mainly on the Arabian Peninsula. As of July 2023, the WHO has recorded 2,605 cases, including 936 deaths from MERS-CoV. There is no vaccine against MERS, and treatment consists of supportive care.43
4.2 Influenza
4.2.1 Avian Influenza, Cambodia
Cambodia has reported four cases of human infections with highly pathogenic avian influenza (HPAI) A(H5N1) virus; three of which were children.44 A 9-year-old boy from the northeastern province of Kratie became the first casualty in 2024. His death was confirmed by the Health Ministry on 8 February, 12 days after the second caseFootnote4. The deceased had presented with fever, shortness of breath, coughing, and fainting after eating a meal made from dead poultry his parents had cooked; investigations revealed that 5 chickens and three ducks they reared had died. His 16-year-old brother who also shared the meal but lives in a different household, tested positive for the virus though symptomless. Close contacts have been identified and administered with antiviral (Tamiflu) to prevent any possible local outbreaks.45 46
4GLOBAL UPDATES ON COVID-19 AND OTHER DISEASES (12 FEBRUARY 2024), Section 5.6.1.
According to Avian Flu Diary, this is the ninth HPAI case reported by the Cambodian authorities in less than a year, as well as “the biggest 12-month total for any nation since 2015”. This is also the fifth fatality at the same time. As with the previous 8 cases, this infection is likely caused by the older 2.3.2.1c clade of the virus. This ‘pocket’ of cases comes after a 9-year quiescence of the H5N1 virus in Cambodia.46
The older clade 2.3.2.1cFootnote5 had successfully spread from Asia to West Africa. Its ‘re- emergence’ in Cambodia could mean that it could “conceivably” pose a threat to nations outside of Cambodia. There has not been any evidence of sustained or efficient human-to- human transmission of H5N1 to date. However, the recent uptick in clade 2.3.2.1c infections warrants attention.46
5 The clade 2.3.2.1c was predominant in the 2009-2010 and 2014-2015 seasons. Newer circulating strains belong to clade 2.3.4.4b. 66
The One Health approach is being used by various agencies in Cambodia as well as the WHO, the United States Agency for International Development (USAID), the Food and Agriculture Organization (FAO), and the Wildlife Conservation Society of Cambodia to collaboratively respond to these sporadic human infections.47
4.2.2 Mortality, New Zealand
Six people have died from influenza A in New Zealand in a space of 12 days recently. They were all from a residential aged care centre in Whitianga (Waikato Region, North Island). The first case was identified on 26 January 2024 and all of the fatalities occurred between 28 January and 8 February 2024. Health New Zealand was notified of the “influenza-like symptoms” outbreak on 28 January 2024. National Public Health Service (NPHS) provided information and guidance for managing the outbreak and declared the outbreak closed on 9 February 2024 based on no further spread of the illness.48
4.3 Cholera, Southern Africa
Southern Africa has a dire cholera situation.49 50
Cholera was on a trend that came to a low in 2020. An uptick began in West Africa in 2021 followed by the current outbreak in the southern part of the continent, likely caused by severe storms and above-normal rains, including floods that destroy infrastructure and add to poor water and sewer systems and the lack of vaccines – a vicious cycle that increases the risk of the disease.51 52 53
The epidemic has since infected > 220,000 people and killed > 4,000 people in 7 countries – the deadliest blow to have hit Africa in terms of cases and deaths in at least a decade. Public health workers in Africa have acknowledged the outbreak as a rare event as it involved many countries at the same time.
According to Zambia health authorities, approximately half of the deaths reported occurred at home rather than at health centres, an indication that people either denied or were unaware they had cholera.54
Representatives from 15 nations in the Southern African Development Community have agreed to a collective mobilisation that includes investing in vaccine production and distribution, collaborating on surveillance for the illness across borders, and developing reliable water and sanitation systems.
Cholera has been a WHO grade 3 emergency since January 2023Footnote 6 – the risk at the global level remains very high.
6 GLOBAL UPDATES ON COVID-19 AND OTHER DISEASES (12 FEBRUARY 2024), Section 5.10.
4.4 Measles
4.4.1 The WHO and ECDC updates
Measles remains an important cause of death among young children globally – despite the availability of a safe and effective vaccine. While there was a 75% decline in the disease globally between 2008-2018, it is still occurring in many developing countries, particularly in parts of Africa and Asia. In 2018, > 140,000 people died from measles, > 95% of which were in countries with low per capita incomes and weak health infrastructures.55 56 57
The COVID-19 pandemic disrupted routine vaccinations against measles globally in 2020 and 2021, leaving millions of children, mainly in low- and low-middle income countries (LMIC), vulnerable. Fifty-one countries, mostly in Africa, experienced large and disruptive measles outbreaks last year, up from 37 in 2022 and 22 in 2021. In 2022, 22 million children worldwide missed their first dose and another 11 million their second dose; cases leapt by 18% to an estimated 9 million, and deaths to 136,000, mostly among children.56
Fanned by misinformation, vaccine hesitancy and mistrust of authorities is a problem – undermining the success of the vaccine. Under-reporting of cases is of concern as the size of the outbreaks and the total number of cases reported could be just “the tip of the iceberg”. Poor health systems, due to lack of funds and staffing, particularly in countries where conflict, droughts, flooding, and malnutrition occur (such as Ethiopia) make children more vulnerable to deadly infection.
Meanwhile, the European Centre for Disease Prevention and Control (ECDC) warned of a continuing rise in measles in the coming months, due to a spike in cases at the end of 2023 that has continued into the new year, suboptimal vaccine coverage, and the approach of the seasonal peak of the virus.58
The disease is an indicator of gaps in a country’s health system. Boosting the resilience of health systems, ensuring public health capacity, and prioritising routine immunisations, especially in poorer countries, are key to preventing outbreaks. High quality surveillance and increasing clinical awareness of health professionals are also important. Focusing on existing diseases is equally as important as looking into Disease X and future pandemics. Global efforts to contain measles outbreaks are under way with GAVI, The Vaccine Alliance, ensuring the delivery of the vaccines to the arms of 38.5 million children in 15 countries worldwide.
Everyone has a role to play in controlling measles: vaccine providers; the government, by making sure sufficient the health workforce is deployed; and the community, which makes sure it overcomes misinformation and encourages vaccine uptake.
4.4.2 Variant that may reduce test sensitivity identified, Europe
Swiss researchers reported the identification of a measles variant with mutations that resulted in a slight loss in polymerase chain reaction (PCR) test sensitivity. It could result in a false negative in samples with a low viral load. The variant has been detected in 18 countries since December 2021. While the numbers seem to be declining, its circulation though continues.59
Italian researchers described five similar detections from Milan and surrounding areas. Viruses were classified as genotype 8, with no clear epidemiologic links between them. Three patients had travel histories that included Uzbekistan, Thailand, and southern Italy. Their findings confirmed that of the Swiss. It helps raise awareness about variant circulation and the potential for reduced sensitivity to diagnostic tests.60
5.0 Implications for Sarawak based on the views of SIDC
The COVID-19 pandemic is not in the past – it is still with us. Long-COVID needs recognition by the general public, employers, and the authorities as it affects society and the economy.61
The SARS-CoV-2 virus, particularly Omicron is continuing to evolve rapidly. In August 2023, BA.2.86 was first reported. BA.2.87 was detected in September 2023 including several other sublineages, such as JN.1, HV.1. It may be harder to keep up with the virus as it changes. Monitoring hospitalisations rather than trying to follow what the new mutations are and checking if neutralisation assays or experiments are done to investigate the functional impact of the mutation continues to be the way to approach to tracking COVID-19.62
Alaskapox virus (AKPV) highlights the potential of zoonotic pathogens jumping species to infect humans. It also highlights the possibility of orthopoxviruses, including the causative agents of smallpox and mpox, to cause devastating outbreaks in human populations worldwide.
Orthopoxviruses (OPVs) are a group of closely related viruses whose genetic variability is thought to contribute to their diverse host range. We will need to anticipate spillover events by identifying hotspots in geographic regions rich with potential OPVs hosts. This can subsequently be used to target wildlife surveillance, particularly related to concerns about the establishment of the these zoonotic viruses beyond its known range.63
Reference
- Fiore, K. CDC’s Tracking a New COVID Variant: BA.2.87.1. MedPage Today https://www.medpagetoday.com/infectiousdisease/covid19/108757?xid=nl_mpt_DH E_2024-02-
15&eun=g1917798d0r&utm_source=Sailthru&utm_medium=email&utm_campaign=Daily Headlines Evening 2024-02-15&utm_term=NL_Daily_DHE_dual-gmail-definition (2024). - CDC Tracks New SARS-CoV-2 Variant, BA.2.87.1 February 9. Centers for Disease Control and Prevention (CDC) https://www.cdc.gov/respiratory-viruses/whats- new/covid-19-variant-update-2024-02-09.html (2024).
- TRACKING SARS-COV-2 VARIANTS. National Institute for Communicable Diseases, South Africa https://www.nicd.ac.za/diseases-a-z-index/disease-index-covid-19/sars- cov-2-genomic-surveillance-update/ (2024).
- South Africa (COVID-19) Dashboard. Updated 18 February 2024. Zoho Analytics https://www.zoho.com/covid/south-africa/ (2024).
- SARS-CoV-2 variant update: BA.2.87.1. https://www.hug.ch/sites/interhug/files/structures/centre_maladies_virales_emerge ntes/Documents/Swiss national SARS-CoV-2 genomic and variants surveillance program/ba.2.87.1_summary.pdf (2024).
- SARS-CoV-2 Sequencing Update 02 February 2024. https://www.nicd.ac.za/wp- content/uploads/2024/02/Update-of-SA-sequencing-data-from-GISAID-02-Feb- 2024.pdf (2024).
- Beusekom, M. Van. Among SARS-CoV-2 variants, Beta had highest death rate, meta- analysis suggests. CIDRAP (University of Minnesota) https://www.cidrap.umn.edu/covid-19/among-sars-cov-2-variants-beta-had-highest- death-rate-meta-analysis-suggests (2024).
- Xia, Q. et al. Case fatality rates of COVID‐19 during epidemic periods of variants of concern: a meta-analysis by continents. Int. J. Infect. Dis. (2024) doi:10.1016/j.ijid.2024.01.017.
- Beusekom, M. Van. COVID Omicron carries 4 times the risk of death as flu, new data show. CIDRAP (University of Minnesota) https://www.cidrap.umn.edu/covid- 19/covid-omicron-carries-4-times-risk-death-flu-new-data-show (2023).
- Goldstein, E. Mortality associated with Omicron and influenza infections in France before and during the COVID-19 pandemic. Epidemiol. Infect. 151, e148 (2023).
- CDC Opens New East Asia and Pacific Regional Office in Japan. at https://www.cdc.gov/media/releases/2024/p0202-cdc-japan- office.html?ACSTrackingID=USCDC_1_3-DM121625&ACSTrackingLabel=CDC Newsroom%3A Week In Review – 02%2F09%2F2024&deliveryName=USCDC_1_3- DM121625 (2024).
- Global Health. CDC’s Regional Offices Around the World. Centers for Disease Control and Prevention (CDC) https://www.cdc.gov/globalhealth/countries/regional/default.htm (2024).
- Sandman, P. M. Why I Hope the COVID Pandemic Isn’t Over. MedPage Today https://www.medpagetoday.com/opinion/second- opinions/108404?xid=nl_secondopinion_2024-01-28&eun=g1917798d0r (2024).
- Data. Monthly Provisional Counts of Deaths by Select Causes, 2020-2023. Centers for Disease Control and Prevention (CDC) https://data.cdc.gov/NCHS/Monthly- Provisional-Counts-of-Deaths-by-Select-Cau/9dzk-mvmi/explore/query/SELECT%250A%2560data_as_of%2560%252C%250A %2560start_date%2560%252C%250A
%2560end_date%2560%252C%250A%2560jurisdiction_of_occurrence%2560%252C%250A%2560year%2560%252C%250A %2560month%2560%252C%25 (2024). - Sawyer, S., Barbachano-Guerrero, A. & Warren, C. Is COVID-19 here to stay? A team of biologists explains what it means for a virus to become endemic. The Conversation https://theconversation.com/is-covid-19-here-to-stay-a-team-of-biologists-explains- what-it-means-for-a-virus-to-become-endemic-168462 (2021).
- Karis, N. The coronavirus could mutate to cause more severe disease, according to experts. Salon https://www.salon.com/2024/01/12/more-severe-disease-symptoms/ (2024).
- Zhang, L. et al. SARS-CoV-2 BA.2.86 enters lung cells and evades neutralizing antibodies with high efficiency. Cell 187, 596-608.e17 (2024).
- Kahn, K. ‘Long Flu’ Is Real — But Long COVID Is Worse, Study Shows. MedPage Today
https://www.medpagetoday.com/infectiousdisease/uritheflu/107898 (2023). - Xie, Y., Choi, T. & Al-Aly, Z. Long-term outcomes following hospital admission for COVID-19 versus seasonal influenza: a cohort study. Lancet Infect. Dis. (2023) doi:10.1016/S1473-3099(23)00684-9.
- Long COVID: East Asia and Pacific Economic Update, October 2021. The World Bank https://www.worldbank.org/en/region/eap/publication/long-covid-east-asia-and- pacific-economic-update-october-2021 (2021).
- Kahn, K. Amid Surge, CDC Unveils New Syphilis Testing Guidance. MedPage Today https://www.medpagetoday.com/infectiousdisease/stds/108655?xid=nl_mpt_DHE_2 024-02-
08&eun=g1917798d0r&utm_source=Sailthru&utm_medium=email&utm_campaign= Daily Headlines Evening 2024-02-08&utm_term=NL_Daily_DHE_dual-gmail-definition (2024). - Papp, J. R. et al. CDC Laboratory Recommendations for Syphilis Testing, United States, 2024. MMWR. Recomm. Reports 73, 1–32 (2024).
- Testing the tests: Scientists seek out best on-the-spot diagnostics for deadly Nipah and Lassa. at https://cepi.net/news_cepi/testing-the-tests-scientists-seek-out-best- on-the-spot-diagnostics-for-deadly-nipah-and-lassa/ (2024).
- Schnirring, L. CEPI and FIND partner to identify best Nipah and Lassa virus rapid tests. CIDRAP (University of Minnesota) https://www.cidrap.umn.edu/lassa/cepi-and-find- partner-identify-best-nipah-and-lassa-virus-rapid-tests (2024).
- Schnirring, L. Alaska reports fatal Alaskapox case. CIDRAP (University of Minnesota) https://www.cidrap.umn.edu/orthopoxvirus/alaska-reports-fatal-alaskapox-case (2024).
- TPOXX. Drugs.com https://www.drugs.com/tpoxx.html (2024).
- Brincidofovir (Oral). Drugs.com https://www.drugs.com/cons/brincidofovir.html (2024).
- Alaskapox virus. Health Alaska, Department of Health State of Alaska
https://health.alaska.gov/dph/Epi/id/Pages/Alaskapox.aspx (2024). - Park, A. A Man Has Died From Alaskapox. Here’s What We Know About the Virus. Time https://time.com/6694518/what-is- alaskapox/?utm_medium=email&utm_source=sfmc&utm_campaign=newsletter+hea lth+default+ac&utm_content=+++20240213+++body&et_rid=240513843&lctg=240513843 (2024).
- Gigante, C. M. et al. Genome of Alaskapox Virus, A Novel Orthopoxvirus Isolated from Alaska. Viruses 11, 708 (2019).
- Newell, K. Alaskapox Virus Infections and Investigation of Zoonotic Sources — Alaska, 2020–2021. in 2023 Epidemic Intelligence Service (EIS) Conference April 24–27, 2023 110 (Centers for Disease Control and Prevention (CDC), 2023).
- Deschutes County confirms case of human plague in local resident. at https://www.deschutes.org/health/page/deschutes-county-confirms-case-human- plague-local-resident (2024).
- Bendix, A. Oregon’s first case of human plague in 8 years likely came from a pet cat. NBC News https://www.nbcnews.com/health/health-news/oregons-first-case- human-plague-8-years-likely-came-cat-rcna138090 (2024).
- Duchamps, L. Oregon Reports First Human Case of Bubonic Plague in Nearly a Decade. The Epoch Times https://www.theepochtimes.com/health/oregon-reports- first-human-case-of-bubonic-plague-in-nearly-a-decade- 5585845?utm_source=newsnoe&src_src=newsnoe&utm_campaign=breaking-2024- 02-14-one&src_cmp=breaking-2024-02-14- one&utm_medium=email&est=AAAAAAAAAAAAAAAA (2024).
- Human Plague cases Oregon, 1934-2024. 1 at https://www.oregon.gov/oha/PH/DISEASESCONDITIONS/DISEASESAZ/Plague1/plagu emap.pdf (2024).
- Maps and Statistics. Plague in the United States. Centers for Disease Control and Prevention (CDC) https://www.cdc.gov/plague/maps/index.html (2024).
- Fact sheets. Plague. World Health Organization (WHO) https://www.who.int/news- room/fact-sheets/detail/plague (2022).
- Plague. World Health Organization/Eastern Mediterranean Region
https://www.emro.who.int/health-topics/plague/introduction.html (2024). - Howard, J. Plague was one of history’s deadliest diseases—then we found a cure. National Geographic https://www.nationalgeographic.com/science/article/the- plague (2020).
- NIAID Emerging Infectious Diseases/Pathogens. National Institutes of Allergy and Infectious Diseases (NIAID) https://www.niaid.nih.gov/research/emerging-infectious- diseases-pathogens (2024).
- Beusekom, M. Van. Researchers identify episodic MERS cases in Kenyan camels, evidence of infection in people. CIDRAP (University of Minnesota) https://www.cidrap.umn.edu/mers-cov/researchers-identify-episodic-mers-cases- kenyan-camels-evidence-infection-people (2024).
- Ogoti, B. M. et al. Biphasic MERS-CoV Incidence in Nomadic Dromedaries with Putative Transmission to Humans, Kenya, 2022–2023. Emerg. Infect. Dis. 30, (2024).
- Middle East respiratory syndrome coronavirus –United Arab Emirates. 2023-DON478. at https://www.who.int/emergencies/disease-outbreak-news/item/2023-DON478 (2024).
- Cheang, S. Cambodia reports a new bird flu case, the brother of a 9-year-old who died of the virus. AP https://apnews.com/article/cambodia-bird-flu-avian-influenza-virus- 4795dcb690b4bb449e4c26a3b49e77dc (2024).
- Cambodia records first ever death from H5N1 bird flu this year; nine-year-old boy the victim. The Star/Xinhua https://www.thestar.com.my/aseanplus/aseanplus- news/2024/02/10/cambodia-records-first-ever-death-from-h5n1-bird-flu-this-year- nine-year-old-boy-the-victim (2024).
- #17,901. Cambodia: MOH Announces 3rd H5N1 Case of 2024 (February 09, 2024). https://afludiary.blogspot.com/2024/02/cambodia-moh-announces-3rd-h5n1-case- of.html.
- First Human Influenza A(H5N1) (Bird Flu) Virus Infections in Cambodia Reported for 2024. Centers for Disease Control and Prevention (CDC) https://www.cdc.gov/flu/avianflu/spotlights/2023-2024/cambodia-human-reported- 2024.htm (2024).
- Kumar, M. Whitianga rest home: Influenza outbreak, six dead. New Zealand Herald https://www.nzherald.co.nz/waikato-news/news/whitianga-rest-home-influenza- outbreak-six- dead/HJUC2B4US5DNTJEOHGJTLUWH6I/?lid=e13fk0anpvo1&utm_source=newsletter &utm_medium=nzh_email&utm_campaign=News_Direct_Morning_Headlines&uuid= 040afc1a8f3040f48be01854bf (2024).
- Eligon, J. & Moyo, J. Deadliest Cholera Outbreak in Past Decade Hits Southern Africa. The New York Times https://www.nytimes.com/2024/02/13/world/africa/cholera- outbreak-zimbabwe-zambia- malawi.html?campaign_id=7&emc=edit_mbae_20240213&instance_id=115085&nl= morning-briefing%3A-asia-pacific- edition®i_id=167497771&segment_id=158104&te=1&user_id=c160e57994afe (2024).
- Multi-country outbreak of cholera, External situation report #11 – 12 February 2024.
Edition 11. 12 February 2024. https://www.who.int/publications/m/item/multi- country-outbreak-of-cholera–external-situation-report–11 12-february-2024
(2024). - Rigby, J. & Dickie, G. Cholera vaccine stocks ‘empty’ as cases surge. Reuters https://www.reuters.com/business/healthcare-pharmaceuticals/cholera-vaccine- stocks-empty-cases-surge-2024-02-14/ (2024).
- Communiqué from Africa CDC on the Southern Africa Development Community (SADC) Extra Ordinary Virtual Summit of Heads of State and Government on the Cholera situation in the region. at https://africacdc.org/news-item/communique- from-africa-cdc-on-the-southern-africa-development-community-sadc-extra-ordinary-virtual-summit-of-heads-of-state-and-government-on-the-cholera-situation- in-the-region/ (2024).
- Interactive summary visuals of cholera data officially reported to WHO since 2000. World Health Organization (WHO) https://www.who.int/activities/supporting- cholera-outbreak-response/interactive-summary-visuals-of-cholera-data-officially- reported-to-who-since-2000 (2024).
- Ministry of Health Zambia (February 13, 2024). National Daily Cholera Update. 12th February 2024. https://www.facebook.com/photo/?fbid=809155874585265&set=pb.100064725786 912.-2207520000&_rdc=1&_rdr.
- Children most at risk as measles cases soar from Ethiopia to Yemen. The Economic Times of India/Reuters https://health.economictimes.indiatimes.com/news/industry/children-most-at-risk- as-measles-cases-soar-from-ethiopia-to- yemen/107711611?action=profile_completion&utm_source=Mailer&utm_medium=n ewsletter&utm_campaign=ethealth_news_2024-02-16&dt=2024-02-16&em (2024).
- Global measles threat continues to grow as another year passes with millions of children unvaccinated. 16 November 2023. at https://www.who.int/news/item/16- 11-2023-global-measles-threat-continues-to-grow-as-another-year-passes-with- millions-of-children-unvaccinated (2023).
- Measles. World Health Organization (WHO) https://www.who.int/health- topics/measles#tab=tab_1 (2024).
- Schnirring, L. ECDC warns of rising measles cases amid vaccination gaps. CIDRAP (University of Minnesota) https://www.cidrap.umn.edu/measles/ecdc-warns-rising- measles-cases-amid-vaccination-gaps (2024).
- Pérez-Rodríguez, F.-J., Cherpillod, P., Thomasson, V., Vetter, P. & Schibler, M. Identification of a measles variant displaying mutations impacting molecular diagnostics, Geneva, Switzerland, 2023. Eurosurveillance 29, (2024).
- Fappani, C. et al. Letter to the editor: Further identification of a measles variant displaying mutations impacting molecular diagnostics, Northern Italy, 2024. Eurosurveillance 29, (2024).
- Wu, K. J. How Much Less to Worry About Long COVID Now. The Atlantic https://www.theatlantic.com/health/archive/2024/01/long-covid-dropping-risk- incidence/677183/ (2024).
- Fiore, K. What to Know About the HV.1 Variant. MedPage Today
https://www.medpagetoday.com/special-reports/exclusives/106885 (2023). - Tseng, K. K. et al. Viral genomic features predict orthopoxvirus reservoir hosts. BioRxiv 17 (2023) doi:https://doi.org/10.1101/2023.10.26.564211.
- Human Development Index (HDI). United Nations Development Programme (UNDP) https://hdr.undp.org/data-center/human-development-index#/indicies/HDI (2024).
- Alaska by Region. Official Alaska State Website https://www.alaska.gov/kids/learn/region.htm (2024).
- Charostad, J. et al. A comprehensive review of highly pathogenic avian influenza (HPAI) H5N1: An imminent threat at doorstep. Travel Med. Infect. Dis. 55, 102638 (2023).